The HOAX of the larvacide-containing “contaminated” water as the “true” source for microcephaly appears to be now put to rest.
Earlier, a HOAX was announced that microcephaly doesn’t come from Zika Virus…it comes from “the larvacide… pyroproxyfen” (correct spelling is: pyriproxyfen) placed in the drinking water at the same locations where both Zika and microcephaly occur. Argentinian and Brazilian scientists of Production Team REDUAS made this assertion on 3 February 2016 in a publication authored by Dr. Medardo Avila Vazquez.
And, it was soon discovered that larviciding is nothing new. In fact, it has been practiced as an effective, WHO-approved method for mosquito control for over 100 years.
The International Health Board (IHB) of 1915 served as current wisdom during the major eradication efforts for Yellow Fever, 100 years ago. According to Frank M. Snowden’s book (2014), “The Global Challenge of Malaria: Past Lessons and Future Prospects,” the IHB 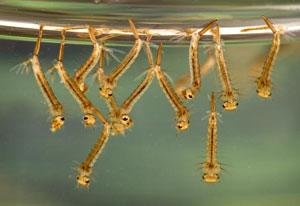 quickly learned that mosquito larviciding was much more effective than chasing adult mosquitoes.
quickly learned that mosquito larviciding was much more effective than chasing adult mosquitoes.
In fact, the IHB advised the Brazilians of that day to abandon all efforts to kill fully grown mosquitos such as fogging and spraying. It recommended, instead, that they focus on reducing the mosquito larvae population, which is much more responsive to minimal effort.
Long-term inattention to larviciding since the initial fight against Yellow Fever has permitted overgrowth of the Aedes (for Dengue and Zika and Yellow Fever) and Anopheles (for Malaria) mosquitoes along the Americas.
So, how has this put to rest the matter of larvicide as the false source for the recent uptick in microcephaly?
The World Health Organization (WHO) reported that two countries, Colombia and Venezuela, are documenting similar spikes in the life-threatening paralysis, the Guillain-Barré syndrome (GBS) (Guillain-Barré syndrome – Colombia and Venezuela, 2016).
Colombia documents 86 new cases of GBS in the past five weeks, which is 3 times higher than normal. “Normal” was based on the past 6 years of statistics in Colombia, which is usually 242 new cases in an entire year. Each GBS case had Zika Virus symptoms.
Venezuela documents 252 new cases of GBS, just in the month of January 2016. Each registered Zika Virus symptoms. Only three (3) of the GBS cases, however, were confirmed Zika-positive by polymerase chain reaction (PCR) test.
There is no vaccination option or specific anti-viral therapy currently available. 65% of the Venezuelan cases had additional complications and received variations of plasmapheresis transfusions and immunoglobulin injections (Guillain-Barré syndrome – Colombia and Venezuela, 2016).
WHO strongly urges people in affected countries to USE larvacides as part of the WHO Pesticide Evaluation Scheme (WHOPES) of 2003 (Najera and Zaim, 2003). And, revised in 2006 (PESTICIDES AND THEIR APPLICATION: For the control of vectors and pests of public health importance, 2006).
Page 80 of the 2003 document “MALARIA VECTOR CONTROL,” outlines approved practices in larviciding. The WHO details petroleum (oil), polystyrene beads, low dose organophosphates and insect growth regulators (pyriproxyfen and diflubenzuron), and microbial insecticides (of the bacterium Bacillus genus) as effective larvicides.
Table 4 on page 29 of the 2006 document outlines the WHO-approved concentrations to treat mosquitoes. “Larviciding should be considered as complementary to environmental management. Page 31 states, “The toxicology of the active ingredients methoprene, pyriproxyfen and temephos and those in B. thuringiensis israelensis has been assessed by the International Programme on Chemical Safety (IPCS) to determine their safety for use as mosquito larvicides in drinking-water at dosages that are effective against Aedes larvae.”
The WHO Guidelines for Drinking Water Quality of 2011 outlines, in Chapter 12.2, safe pesticide use for drinking water sources (Guidelines for drinking-water quality, 2011). Pyriproxyfen is documented on page 439-40 of Chapter 12.2 (Chemical fact sheets, 2011).
“WHO has assessed pyriproxyfen for use as a mosquito larvicide in drinking-water in containers, particularly to control dengue fever. The recommended dosage of pyriproxyfen in potable water in containers should not exceed 0.01 mg/l under WHOPES.”
REFERENCES:
Avila Vazquez, M. (2016). REPORT from Physicians in the Crop-Sprayed Villages regarding Dengue-Zika, microcephaly, and mass-spraying with chemical poisons. Team REDUAS. Retrieved February 15, 2016 from http://www.reduas.com.ar/wp-content/uploads/downloads/2016/02/Informe-Zika-de-Reduas_TRAD.pdf
Chemical fact sheets. (2011). Chapter 12, Guidelines for drinking-water quality, fourth edition. Water Sanitation Health. World Health Organization. Retrieved February 16, 2016 http://www.who.int/water_sanitation_health/publications/2011/9789241548151_ch12.pdf?ua=1
Guidelines for drinking-water quality, fourth edition. (2011). Water Sanitation Health. World Health Organization. Retrieved February 16, 2016 from http://www.who.int/water_sanitation_health/publications/2011/dwq_chapters/en/
Guillain-Barré syndrome – Colombia and Venezuela. (2016). Disease Outbreak News, January 12, 2016. World Health Organization. Retrieved February 16, 2016 from http://www.who.int/csr/don/12-february-2016-gbs-colombia-venezuela/en/
Najera, J.A. and Zaim, M. (2003). MALARIA VECTOR CONTROL: DECISION MAKING CRITERIA AND PROCEDURES FOR JUDICIOUS USE OF INSECTICIDES. WHO Pesticide Evaluation Scheme (WHOPES). Retrieved February 16, 2016 from http://apps.who.int/iris/bitstream/10665/67365/1/WHO_CDS_WHOPES_2002.5_Rev.1.pdf
PESTICIDES AND THEIR APPLICATION: For the control of vectors and pests of public health importance. (2006). 6th edition. Department of Control of Neglected Tropical Diseases. WHO Pesticide evaluation scheme (WHOPES). Retrieved February 16, 2016 from http://apps.who.int/iris/bitstream/10665/69795/1/WHO_CDS_NTD_WHOPES_GCDPP_2006.1_eng.pdf
Snowden, F. M. and Bucala, R. (2014). The Global Challenge of Malaria : Past Lessons and Future Prospects. Singapore: World Scientific Publishing Company. ISBN: 978-9814405584 9814405582.